Surgery
Surgery for cancer of the head of pancreas
Surgery provides the only opportunity for cure in patients with pancreatic cancer. Unfortunately only 10-15% of patients will have operable disease. Accurate pre-operative staging is important so that patients with inoperable or incurable disease avoid unnecessary major abdominal surgery. Involvement of the abdominal vessels supplying the gut or other organs in the abdominal cavity, may well represent a contra-indication to surgery.
Removal of tumours from the head of the pancreas is done by an operation called a pancreatico-duodenectomy (Kausch-Whipple procedure). This operation involves removal of the lower half of the stomach, the duodenum, the gall bladder and lower bile duct, the head, uncinate process and neck of pancreas. Reconstruction requires several different joins to the small intestines.
Whipple resection in stages (click images to enlarge)
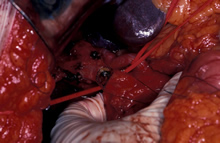 Division of the common hepatic (bile) duct |
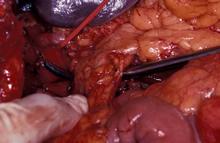 Instrument under the neck of the pancreas |
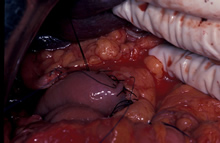
 Division of the neck of the pancreas and retraction of head of pancreas to the right exposing SMA |
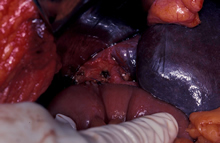
 Completed Whipple resection specimen |
 SMA shown, skeletonised and cleared |
 Pancreato jejunostomy anastomosis (join up) |
 Hepatico jejunostomy anastomosis (join up) |
 Gastro jejunostomy anastomosis |
 Gastro jejunostomy anastomosis completed |
In some patients with small tumours of the end of the bile duct the outlet of the stomach may be preserved and a Pylorus-Preserving Pancreato-Duodenectomy (PPPD) is carried out. This operation has the advantage of preserving the whole stomach with an improvement in post-operative quality of life. The problem with PPPD is that some patients have prolonged gastric (stomach) emptying leading to a need for intravenous feeding and a nasogastric tube for a few days. Following a conventional Whipple operation recovery is usually faster.
Risks of Whipple and PPPD Resections
The published operative mortality for pancreatico-duodenectomy can be up to 5% in Specialist Centres. Presently it is < 3% in Prof Karanjia series and this is similar to figures from other high volume centres. Some patients may require a blood transfusion either at the time of surgery or post-operatively. Approximately 5% of patients may develop a complication which may necessitate their return to the operating theatre. Approximately 7% of patients may develop a leak of pancreatic juice from the join between the pancreas and small intestine (a pancreatic fistula). Mostly these fistulae settle with conservative management - prolonged tube drainage.
A proportion of patients who are not diabetic pre-operatively will become diabetic post-operatively. Those who are already Type 2 diabetics pre-operatively may become insulin dependent afterwards.
Many patients develop pancreatic exocrine insufficiency. This means that they cannot make sufficient pancreatic juice and enzymes to digest their food and consequently they do not absorb nutrients from their food. These patients are at high risk of malabsorption with consequent steatorrhoea (fatty greasy stools). This is best corrected by oral pancreatic extract with meals in the form of Creon capsules.
Surgery for cancer of the body and tail of the pancreas
For tumours that involve the body and the tail of the pancreas, a left sided or distal pancreatectomy is performed. This involves removal of the body and tail of pancreas together with spleen and surrounding lymph node tissue. In selected patients this procedure is amenable to a laparoscopic or keyhole approach.
 |
CT scan showing tumour in the tail of the pancreas. |
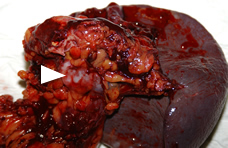 |
Operative photograph of tail of pancreas and spleen following distal pancreatectomy. |
Risks of Distal Pancreatectomy
The operative mortality for distal pancreatectomy should be less than 2-3% in Specialist Centres. Presently it is 3% in our centre and this is similar to figures from other high volume centres. Up to 20% of patients may require a blood transfusion either at the time of surgery or post-operatively. Approximately 7-10% of patients may develop a leak of pancreatic juice from the closed stump of pancreas (a pancreatic fistula). Mostly these fistulae settle with conservative management - prolonged tube drainage. Occasionally patients may need an ERCP and pancreatic sphincterotomy or pancreatic ductal stenting.
As splenectomy is performed patients are also at risk of post splenectomy sepsis and require long term prophyllaxis with Penicillin V tablets (or erythromycin if penicillin allergic). Patients should have had pre-operative vaccinations with Pneumovax, Meningovax and Haemophilus Influenzae vaccines. Patients are at risk of developing a high platelet count after splenectomy and they may require to have long term asprin.